
Dr. Rajat Sachdeva MDS
Cosmetic & Implant Dentist | Microscope-Assisted Digital Dentistry | Smile Design Expert23 Years of experience
Introduction
Maintenance of gingival health is one of the keys to the longevity of teeth as well as the durability of restorations.
In this context, the biologic width functions as a natural protective barrier against the entrance of microorganisms into the periodontal ligament, gingival connective tissue, and alveolar bone.
An adequate understanding of the relationship between periodontal tissues and restorative dentistry is paramount to ensure proper form, function, esthetics, and comfort of the dentition. While most clinicians recognize this critical relationship, uncertainty often remains regarding specific concepts such as the biologic width and the placement of restorative margins.
But what exactly is the biologic width? Why, despite best efforts to esthetically hide a crown margin within the sulcus, does it sometimes reappear or cause inflammation at follow-up visits?
Understanding the Biologic Width
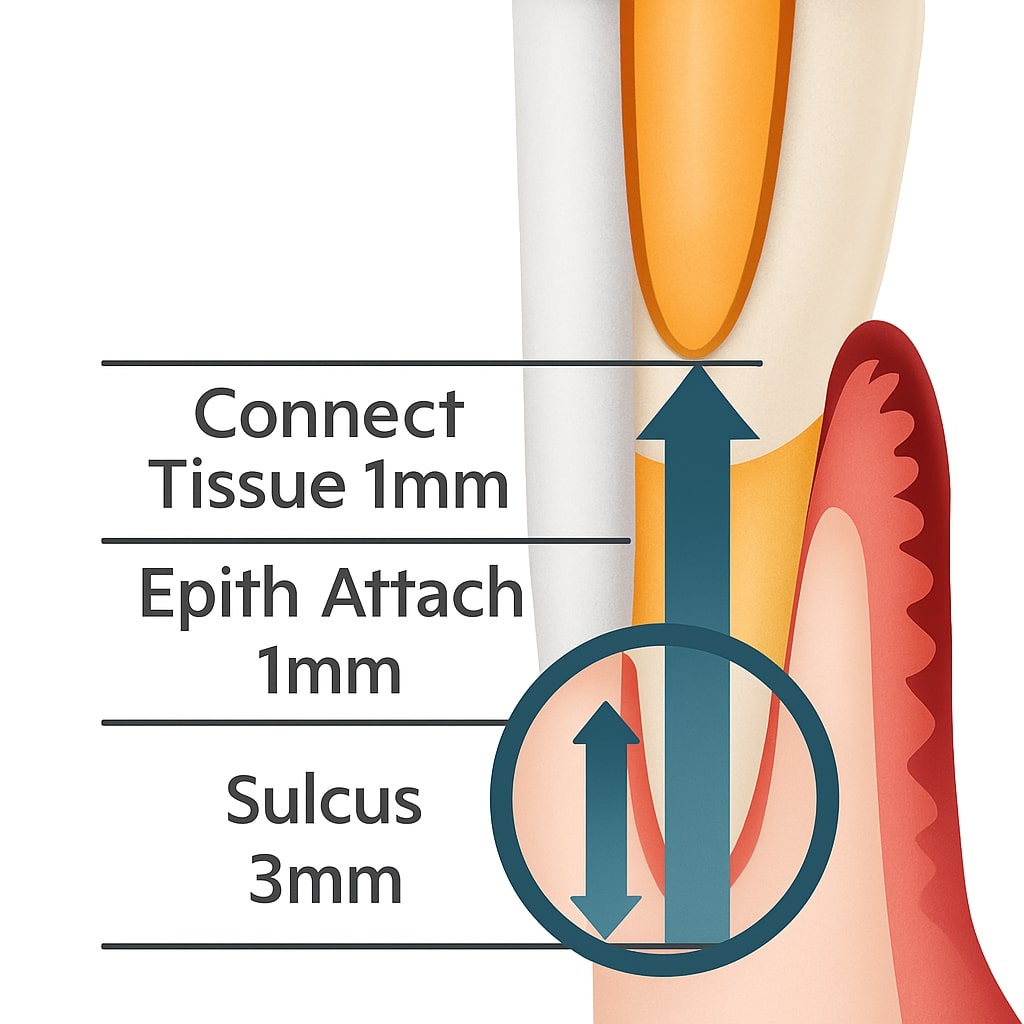
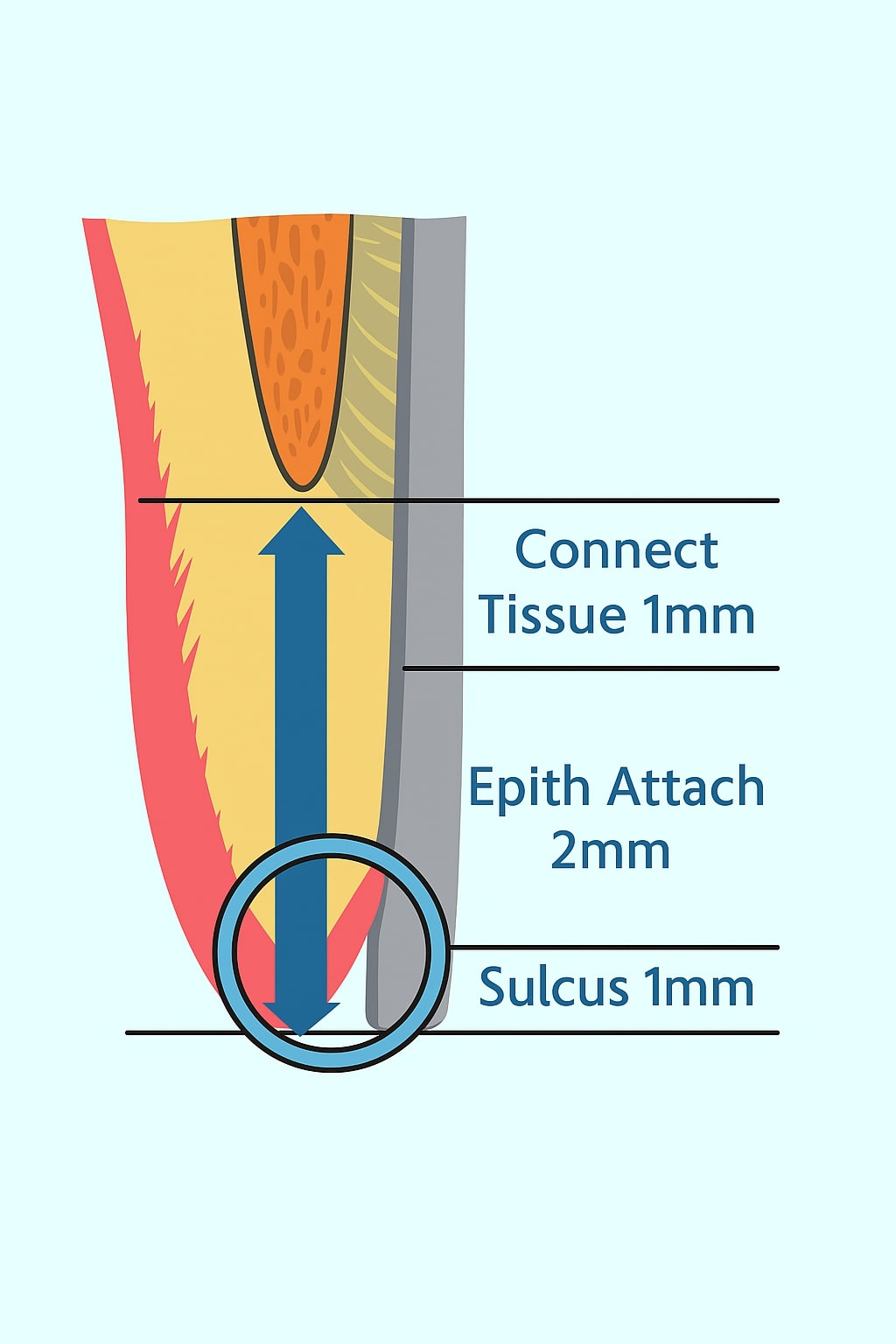 The biologic width is the combined height of the epithelial attachment and connective tissue attachment above the alveolar bone — approximately 2 mm.
The biologic width is the combined height of the epithelial attachment and connective tissue attachment above the alveolar bone — approximately 2 mm.
Including the sulcus depth (around 1 mm), this results in an average 3 mm distance from the alveolar crest to the gingival margin.
This natural dimension serves as a defensive zone that protects the periodontal tissues and maintains stability.
Violation of this width — by placing a restorative margin too close to or within this area — can lead to:
- Chronic inflammation
- Loss of attachment
- Bone resorption
- Gingival recession
Therefore, proper margin placement is essential not only for esthetics but also for long-term periodontal and restorative success.
Supragingival vs. Subgingival Margins
Supragingival margin placement is the location of choice for restorative margins to avoid iatrogenic periodontal disease. It allows for:
- Easier finishing and polishing
- Better plaque control
- Reduced risk of biological width violation
In certain cases, however, subgingival margin placement becomes necessary. When this is required, consideration of key biological and clinical factors helps reduce adverse effects on periodontal tissues.
From a periodontal viewpoint, both supragingival and equigingival margins are well tolerated when properly designed.
Why Subgingival Margins Are Needed
Subgingival margin placement is sometimes indicated to:
- Mask tooth discoloration
- Hide restoration margins for a seamless appearance
- Manage deep caries or replace existing restorations extending below the gingiva
- Increase tooth structure for better retention and resistance
However, incorrect placement can lead to serious complications such as:
- Violation of the biologic width
- Gingival inflammation
- Soft tissue recession
The Importance of Sulcus Depth Awareness
When treatment planning for subgingival margin placement, awareness of the sulcus depth is crucial.
Knowing how to prepare and where to position margins determines whether the final result will be predictable and esthetic or lead to biologic complications.
Clinical Guidelines for Safe and Predictable Margin Placement
When the Probing Depth Is 1.5 mm or Less
 If the sulcus depth is 1.5 mm or less, extend the margin 0.5–0.7 mm below the tissue level.
If the sulcus depth is 1.5 mm or less, extend the margin 0.5–0.7 mm below the tissue level.
- The risk of gingival recession is minimal because the tissue won’t recede into the biologic attachment.
- Placing the margin deeper than this range may invade the attachment zone and cause inflammation.
- Even if the tissue is removed up to bone level, it will generally re-establish a 1 mm sulcus
Thus, extending 0.5–0.7 mm below tissue achieves optimal esthetics and biological safety.
When the Probing Depth Is Greater Than 1.5 mm
If the sulcus depth exceeds 1.5 mm, place the margin half the depth of the sulcus below the tissue (e.g., in a 3 mm sulcus, place the margin 1.5 mm below).
Alternatively, perform a gingivectomy when esthetically and clinically acceptable to reduce the sulcus depth to 1–1.5 mm.
- Deeper sulci carry a higher risk of recession because of the presence of unattached tissue above the attachment zone.
- Thin biotypes are especially prone to losing sulcus depth and exposing restoration margins over time.
- If gingivectomy is not possible, placing the margin halfway into the sulcus ensures biological safety and esthetic stability.
Simplified Rules for Margin Placement
- If the sulcus probes ≤ 1.5 mm, place the restorative margin 0.5 mm below the gingival crest.
- If the sulcus probes > 1.5 mm, position the margin half the sulcus depth below the tissue.
- If the sulcus is greater than 2 mm, perform a gingivectomy to create a 1.5 mm sulcus.
When to Avoid Subgingival Margins
Teeth with subgingival caries, fractures, or short clinical crowns may lack sufficient coronal tooth structure for proper restoration. In these cases, rather than encroaching on the biologic width, consider:
- Crown lengthening
- Apically repositioned flap with bone recontouring
- Orthodontic extrusion
Gingival Recession Complications
Improper margin placement and biologic width violation can lead to gingival recession, causing both esthetic and functional problems such as:
- Loss of interdental papillae, forming unaesthetic black triangles
- Altered speech due to air escape through interproximal spaces
- Increased plaque accumulation and food lodgment
- Root sensitivity and increased risk of root caries
These complications affect the smile line, phonetics, and overall comfort, emphasizing the need for biologically sound restorative techniques.
Clinical Insight
- Thicker gingival biotypes tolerate deeper margins better and show minimal recession.
- Thin biotypes are more susceptible to attachment loss if margins are placed too deep.
- Supragingival or equigingival margins are safest whenever possible.
- When esthetics demand subgingival extension, always evaluate sulcus depth and biologic width carefully.
Conclusion
The relationship between periodontal health and restorative dentistry is intimate and inseparable. The biologic width is essential for preserving periodontal health, which depends on properly designed restorations.
When possible supragingival margins should be preferred.
If margins must be placed near the alveolar crest, crown-lengthening surgery or orthodontic extrusion should be considered to provide adequate tooth structure while maintaining biologic width integrity.
Although individual variations exist, minimum of 3 mm should exist between the restorative margin and alveolar bone — 2 mm for biologic width and 1 mm for sulcus depth — to ensure periodontal stability and long-term success.
By honoring the biologic width and periodontal architecture, we create results that are not only visually pleasing but also biologically sustainable — protecting our patients’ smiles for the long term.